Q: Can you tell us the background that led you to consider 3D printing as a possible solution for skull implants?
Joel Brie answer: I do very specific craniofacial skeletal reconstruction, with specific shapes. We had a lot of trouble reconstructing the shape perfectly. 3D printing allowed us to access custom parts and so when Christophe Chaput (3DCeram CEO) came to present us the project, it was a very strong expectation for us to have custom parts that have the ideal shape.

Q:When did you start with 3D printing ceramics and what were the steps?
Joel Brie answer: We started in 2005. To be able to bring an implantable medical device to market it’s necessary to go through several stages. You basically have clinical trials. The first one is to check the feasibility. In fact, the first phase will validate the process and the possibility of using it to corroborate the fact that it can give good results. And then, we must move on to an additional step which is the effectiveness study for which we have to increase the number of patients to reach an absolute proof of efficacy. Once we have passed this feasibility study, then there was a request for the CE marking. While we were obtaining the CE marking, we continued, after the preliminary study, to accumulate cases to study up to 24. So we have some insights, we were able to produce evidence of the effectiveness and the safety. Out of the 24 cases, there was no skull implants removal because of infections nor complications until now actually.

Q:What are the indications to this type of prothesis ?
Joel Brie answer: For me, the main indication is very large losses of bone substance that cannot be filled with the patient's own bone. For the skull, it is essentially the cranium-plastie, in other words, a loss of bone substance of the cranial arch which will be greater than 100 square centimeters. We can say that up to 100 square centimeters, we can manage with other processes that are real acceptable choices like autologous cranioplasty or titanium grids with hydroxyapatitel cement. Past 100 square centimeters the custom prosthesis is absolutely essential. After that, there are the 25 to 100 square centimeters segment where you can use both solutions. You can use either the custom prosthesis or other systems. But the custom-made prosthesis is the best, it gives better results. And beyond 100 square centimeters, I mean ten by ten, an hemi-cranium, after that you can't reproduce the volume, mechanical constraints appear, and you can’t avoid custom prosthesis
Q: What are the pathologies leading to this type of surgery ?
Joel Brie answer: The most frequent indication is going to be the flaps of the compressive that are not going back into place. It is a head trauma with the increase in intracranial pressure which causes a cerebral edema that develops after the trauma. So, you have to remove part of the skull vault, so that the brain can expand and be kept from suffering. To save the patient, it is necessary to remove up the skull arch. It could go to an hemi-skull. The decompressive flap can be very large and they are put at the bank of tissues and saved with the idea to be implanted when the edema will have disappeared.

Q:How long after it is ?
Joel Brie answer: Maybe several months. Once the brain is back in its place we will try to put it back. The problem is that at the bank of tissues, the flap is eventually contaminated during the manipulation to storage it. Samples are collected before replacing the skull vault and it happens that the liquid in which it was stored is contaminated, then it cannot be used.
What are the advantages of ceramics over other materials that are available and proposed today for skull implants ?
Joel Brie answer: It's very easy as of today, there are three main families of biomaterials: first generation, second generation and third generation.
To put it simply, first generation biomaterials are bio-inert materials, meaning that the organism accepts them, but there is no interaction between the material and the organism, no osteo integration. The second generation materials will interact with the living environment, for example, the osteo-induction is a of second generation implant property. That means that we are able to induce bone manufacturing of by interaction with the body. So this is the characteristic of calcium phosphate and all materials based calcium and phosphate, like Hydroxyapatite, phosphate tricalcium, biphasic, etc.. These are the materials of second generation.
So if we create porous parts there will be a colonization of the implant by bone tissue. With polymer materials, there is no colonization of the implant. The implant is massive, it is placed and it is firmly fixed to the bone, but there is no bio-integration of the implant as such. So there is a bigger risk of a rejection, infections that are much more important because the implant is rigidly fixed with some plates that are a little thick, and it will never be considered as an element of the body. It will never be truly bio-integrated.
The first cranioplasties were done with polymethyl methacrylate cement. This is the cement that is used to seal hip prostheses in orthopedics with a failure rate reaching 20%, because of infectious problems.
I just took one out that had been there for 20 years. The patient came in with implant bear skinned. All the skin had been destroyed over the implant and in fact the implant was out in the open.
Q: On implants 3D printed with 3DCeram have you had any cases of rejection?
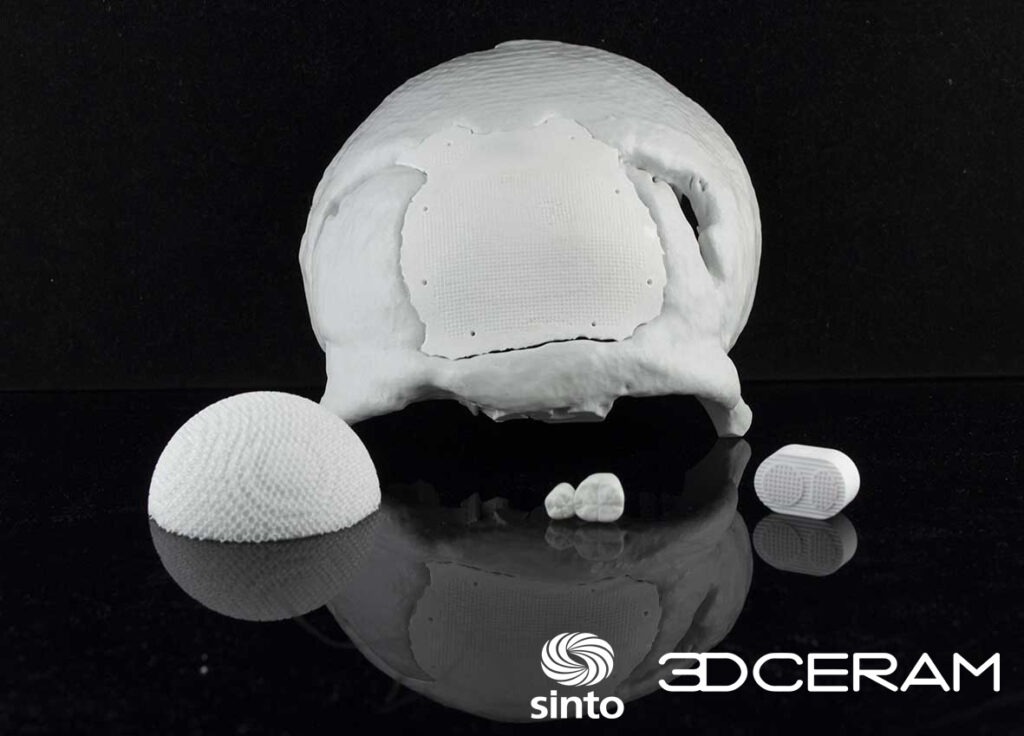
None. The implant that we were using has a rather particular structure, since we know very well that the colonization of an implant is limited, it does not go all the way to the bottom. If the implant is very massive, the colonization by bone tissue will take place over the first centimeter, but not beyond. So, with this in mind, we decided to have a porous part at the periphery, to make the link with the living bone tissue. This is what you can see very clearly between the fixation holes. This prosthesis is perfect as there is a dense part in the middle, with a surface porosity that is important enough for the soft tissues to be able to attach to the prosthesis. After that, there are the dense parts here in the periphery, which were the place of the fixation holes of the prosthesis and between the fixation holes there is a porous area. In fact, in the study that we did, after one year 75% of the periphery was bounded. You could see very clearly the fusion between the surrounding bone tissue and the prosthesis.
There is a primary fixation that was done with absorbable sutures and the secondary fixation of the implant was the result of this osteointegration, of these bone bridges that were created, so the implant was perfectly stable and was perfectly integrated.
When you have a polymer implant, you do not have a bone/implant bond, you have a membrane that forms between the two. The stability is just due to the system of fixation, the plates and screws that holds it in place, so there can be micro movements. We know very well that those micro movements at the interface between the implants and the native bone are causing rejections.
Reconstructing the skull , is not only a cosmetic or protective function, actually it improves the functioning of the brain. We call that the skin flap syndrom. When there is no bone, the air pressure is exerted directly on the brain. To rebuild the skull bone improves cognitive function and more generally the brain function. This patient who was almost no longer speaking after a stroke. It was a semi-skull, frontal, parietal, occipital, that was 150 square centimeters. It was huge ! She was in wheelchair and she was no longer speaking. Her husband came in consultation and explained to me that while he had his lunch with his wife she said two words, that was about green beans, I think, it's too salty. Those were her first words. It seems that the prosthesis improved the functioning of her brain. And beside, she could not walk anymore but she started to take a few steps in the corridor.
Q:What about Titanium implant ?
Considering the forehead, there is no questionning, it’s impossible to get the same result. As long as it not possible to have the thin parts we can get with ceramics on the external part of the implant. It's really continuous. The titanium plates there's 2 mm of thickness, so you can feel the screws through the skin of the forehead. It's a very thin skin. That's why this technology is superior to the Italian technology, which was a molding technology where there were no thin parts. They were molding the loss of substance, but there was a break in continuity between the implant and the native bone. So there was a patient where you could clearly see the shape of the implant because the skin had slipped into this gap, so it was making a groove. With titanium, you have a 2 mm overhang with such an overhang there will be a little stair step that's not big, but the skin is going to follow the stair step and so you're going to feel the screws, the are very unhappy because of this.
There is some titanium ion release on the periphery which are causing an inflammatory reaction around the implant, so they have all been removed. Because in fact, the titanium ion are very inflammatory. So you have inflammation of the bone which resorbs around the implant and as it is big screw, if you lose your the screw thread.
Q:And with ceramic skull implants ?
We were putting resorbable sutures, that went through a hole so there was no perception of any material. That is why the result was close to perfection. Because we had these thin parts, because we had this osteo integration, because the fixation material was not perceptible at all. And if you open back, you will only have the implant, the bone and you have a perfect continuum between the implant and the bone. In the long term, I'd love to see what happens. I have the feedbacks of my neurosurgeon colleagues, and they are not very happy with the titanium prostheses…
Watch the video: "3D Printed and implanted, the story of the first ceramic skull implant"